What Is Pulpitis?
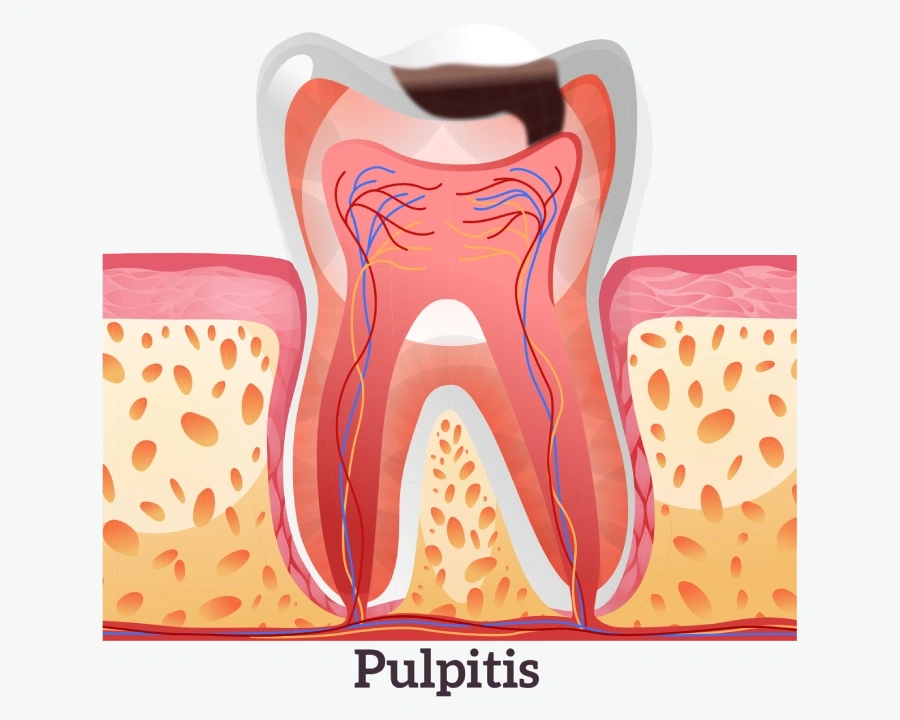
Pulpitis is an inflammation within the tooth pulp. The pulp is connective tissue filling the inner part of the tooth and root canals. It's known as a vascular-nerve bundle due to the abundance of blood vessels and nerves.
The pulp nourishes the tooth, supports its functionality and viability. At the top of the tooth root, there's an opening connecting it to an artery, from which the tooth receives nutrients.
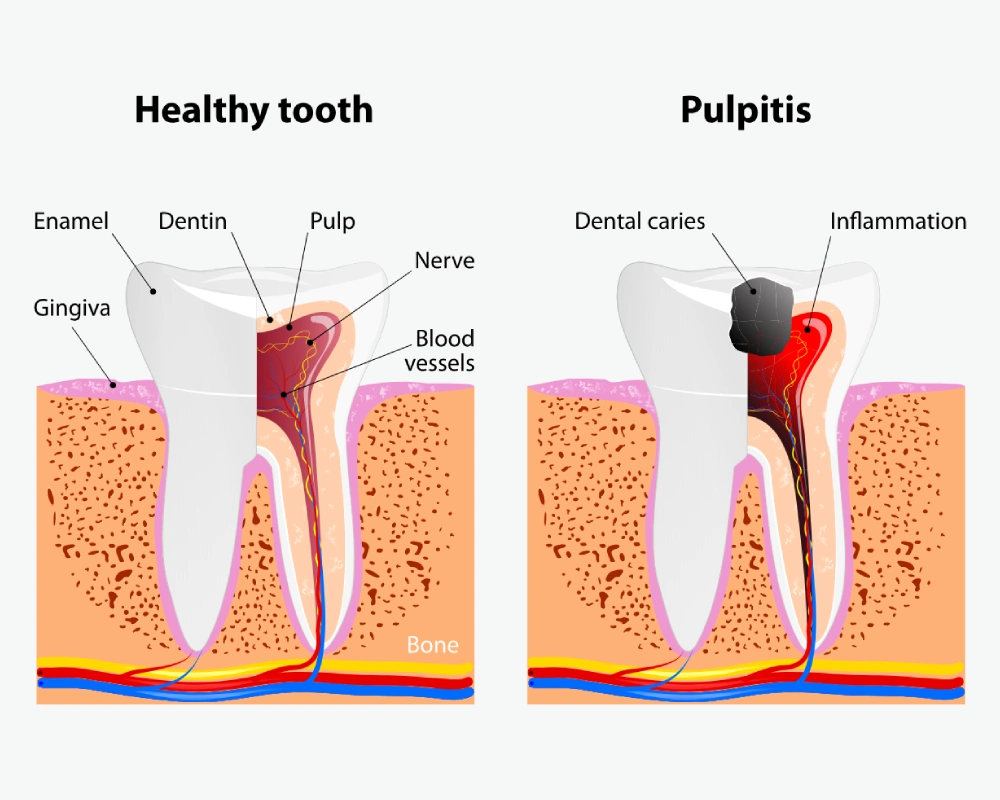
The pulp is located in the center of the tooth, filling the space that mirrors its shape. Its part in the crown area is situated in the cavity of the crown, while the root part is in the root canals. A layer of dentin is located above the pulp, topped with enamel.
Causes
- Deep caries are the primary cause. Bacteria, including streptococci and staphylococci, multiply, attack the enamel, and reach the pulp, causing its inflammation.
- Chronic periodontitis can lead to the infection penetrating the pulp through the dentin tubules.
- Injuries, including tooth fractures, can damage the pulp.
- Improper dental treatment can cause inflammation of the pulp due to inadequate canal treatment or thermal damage.
- Infections spreading through the bloodstream can reach the pulp.
Indicating Symptoms
- Sharp pain that intensifies at night (acute form).
- Pain while chewing, accompanied by gum bleeding and unpleasant odor (hypertrophic pulpitis).
- Darkening of the enamel, gum swelling, enlarged lymph nodes (gangrenous form).
- Prolonged reaction to temperature (focal pulpitis).
- Indeterminate pain location, radiating to the temple, ear, or neck (diffuse form).
- General malaise and aching pain (chronic form).
What Complications Can Pulpitis Cause?
Untreated pulpitis can lead to the following complications:
- Periodontitis. Inflammation of the tissue holding the tooth in the jaw. The infection from the pulp spreads to the tissue around the root, causing inflammation and potential tooth loss.
- Abscess. A purulent inflammation at the tooth root that can spread throughout the body and may require tooth removal.
- Periostitis or flux. Deep infection causing inflammation of the periosteum, swelling of the gum and cheek, fever.
- Osteomyelitis. Infectious inflammation of the jawbone, that destroys bone tissue and can lead to severe complications.
- Sepsis. Spread of infection in the blood, causing severe poisoning and potentially fatal outcomes.
- Cysts. Growths on the tooth roots caused by bacteria from the root canals, can lead to tooth loss.
To alleviate pain, you can take painkillers and use antiseptic mouth rinses. This is a temporary solution, and a visit to the dentist is necessary to avoid serious complications.
Acute
Acute pulpitis causes severe, sudden pain, especially at night. The enamel darkens, and a dark hole eventually reaches the tooth's root canals. The inflammation affects the vascular-nerve bundle, and the disease remains acute for a week.
- Focal: Pain lasts two days, with episodes of sharp pain every 2-3 hours. The gum swells, and the pain is precisely localized.
- Diffuse: Starting on the third day, the entire pulp becomes inflamed. Throbbing pain spreads across the jaw, making it difficult to identify the painful tooth. The pain intensifies and lasts longer.
- Purulent: Unbearable throbbing pain. The affected tooth fills with pus, and the patient's condition worsens.
Traumatic
Traumatic pulpitis results from an injury, such as during sports activities. Saliva and bacteria enter the pulp through chips, causing inflammation.
Chronic
Chronic pulpitis develops without treatment of acute pulpitis. The pain becomes bearable and periodically worsens.
- Fibrous: Aching pain increases with temperature stimuli. The enamel of the tooth becomes dull, fibrous tissue grows in the pulp.
- Gangrenous: Nerve fibers in the pulp die, the crown-like part disintegrates, causing unpleasant mouth odor.
- Hypertrophic: A polyp forms in the pulp chamber, the gum may bleed, the tooth cavity is opened and connects with the carious cavity.
Under the Filling
Occurs when:
- An infection penetrated the tooth due to periodontitis or periodontosis.
- The dentist did not remove all affected tissues before filling. This leads to destruction under the filling and inflammation of the pulp.
- There was no cooling of the tooth tissue with air or water during the filling process, causing damage.
Under the Crown
Develops if:
- Carious tissue was not completely removed before placing the crown.
- Insufficient cooling was provided while grinding the tooth, leading to thermal damage to the pulp.
Pulpitis under the crown develops gradually. If symptoms appear, the crown must be removed, the root canals treated, and a new crown placed.
Retrograde
Develops due to periodontitis. Pathogenic bacteria from deep periodontal pockets penetrate the pulp through the apical openings, causing inflammation.
Three-Canal
Involves molars with three root canals. The inflammation of the pulp in these teeth requires treatment of each canal due to the presence of the vascular-nerve bundle.
Diagnostic Methods for Pulpitis
Successful treatment of pulpitis starts with an accurate diagnosis and identification of the cause. The dentist develops a treatment plan based on the form of pulpitis.
How is the diagnosis conducted?
-
Probing: Using a probe and mirror, the dentist examines the oral
cavity. This method allows assessing:
- Presence and depth of caries;
- The condition of the tooth;
- Mobility of the tooth;
- Condition of the periodontium and depth of periodontal pockets.
- Thermo Diagnosis: The tooth's response to heat and cold is tested. Patients experience prolonged pain from temperature stimuli.
- Electro Odonto Diagnosis (EOD): A weak electric current is directed at the tooth to measure the pulp's sensitivity. The indicators range from 20 to 60 µA.
- Apex location of the root canal: Measuring the canal length with an apex locator. The procedure helps accurately determine the canal length for cleaning and filling.
-
X-ray: A detailed image of the tooth and surrounding tissues allows
identifying:
- The fit of the filling;
- The size of the carious cavity;
- The width of the periodontal gap.
X-ray images reveal inflammations and disorders not visible during a routine examination.
How is Pulpitis Treated?
With Nerve Preservation
This method is chosen when the patient seeks dental care at the first signs of inflammation, such as with acute or traumatic pulpitis. It is most often used for individuals under 30 years of age.
1. Biological Treatment – complete preservation of the pulp.
Steps:
- The dentist administers anesthesia.
- Affected dentin is removed.
- The carious cavity is treated with an antiseptic.
- Antibiotics are applied.
- A temporary filling is placed.
- After a few days, a permanent filling is inserted.
2. Vital Method – partial preservation of the pulp, only its upper part is removed.
Steps:
- The procedure starts with anesthesia.
- The carious cavity is cleaned.
- The cavity is treated with anti-inflammatory agents.
- The upper part of the pulp is removed.
- A healing paste is applied.
- A temporary filling is placed.
- Then, a permanent filling is secured.
With Pulp Removal
This method is used in most cases of treatment.
1. Surgical Treatment – complete removal of the pulp.
Steps:
- Anesthesia is performed.
- Caries is removed.
- A paste is applied that causes the pulp to die.
- Mechanical cleaning and medicinal treatment of the canals.
- The canals are filled.
- The tooth is restored with a temporary and then a permanent filling.
The pulp contains blood and lymphatic vessels, nerve endings, and connective tissue that provide blood supply and mineralization of the tooth. After the removal of the pulp (depulpation), these processes stop, leading to darkening of the tooth and a reduction in its lifespan.
To avoid removing the pulp, it is crucial to treat pulpitis promptly! You should immediately consult a dentist at the first signs of pain.
Prevention of Pulpitis
To prevent pulpitis, it is recommended to:
- Brush your teeth thoroughly twice a day.
- Rinse your mouth after eating.
- Avoid using toothpicks to prevent gum injury.
- Visit a dentist twice a year for preventive measures.
- Timely and properly treat caries and other dental diseases.
- Choose experienced dentists to avoid medical errors.
- Regularly undergo professional teeth cleaning to remove plaque and tartar.
- Consume sufficient vitamins and minerals.
- Avoid smoking to prevent the formation of pigmented plaque and reduce the risk of caries and gum infections.
- Monitor gum health, use special toothpaste if they are sensitive. If your gums are red and bleeding, you need to see a doctor immediately.
- Change your toothbrush every three months.
Frequently Asked Questions
What is the difference between pulpitis and periodontitis?
Pulpitis: The pulp (nerve) becomes inflamed. It is localized inside the tooth. The pain is sharp and severe. There is no mobility of the tooth.
Periodontitis: The periodontium (the space between the bone tissue and the tooth) becomes inflamed. The inflammation develops in the gingival tissues. The pain is aching, intensifying when the jaws are closed. It leads to loosening and loss of the tooth.
Are there any special considerations for treating pulpitis in a baby tooth?
Generally, the treatment approach for diseases in baby teeth is the same as for permanent teeth, albeit more gentle and cautious. Patience is required, as multiple visits to the dentist may be necessary. The dentist will choose the best treatment method for pulpitis in a child after examination and diagnosis.
Some parents think baby teeth do not need treatment because they will fall out. However, if left untreated, the carious process may spread to adjacent teeth or affect the development of future permanent teeth.
Is it painful to treat pulpitis?
No. Before drilling the tooth, the dentist administers local anesthesia. The gum is injected with a pain relief medication. A few minutes after the injection, the patient feels no pain, only pressure. Sedation (a semi-conscious, relaxed state) is also used.
What should I do if my tooth hurts after pulpitis treatment?
For severe tooth pain after pulpitis treatment, you can take pain relievers, rinse your mouth with an antiseptic, or a warm herbal infusion (lemon balm, sage, oak bark, chamomile, calendula). Do not heat the sore tooth, apply alcohol or garlic compresses to the gum, take antibiotics or aspirin. It is better to seek help from a dentist as soon as possible to avoid possible complications.
How long does pulpitis treatment take?
Treatment may require one or several visits to the dental clinic, depending on the complexity of the case.
Can I drink alcohol after pulpitis treatment?
You should avoid alcohol after treatment until your doctor says it is safe.