What Is Meant by Non-Integration or Rejection of an Implant?
- Non-integration of an implant occurs when it fails to bond with the bone within 3-6 months after its placement;
- Rejection of an implant happens when, after a successful union of the artificial root with the jawbone (3-5 years after placement), the connection is lost and the implant becomes unstable.
There are differences between non-integration and rejection of a tooth. The risk of non-integration is 1-2%, while the risk of rejection is 4-5%.
In the short term of (up to 6 months after placement), non-integration of the titanium root is discussed. In the long term (from 2 to 5 years), rejection is discussed.
How Does the Integration of a Tooth Occur?
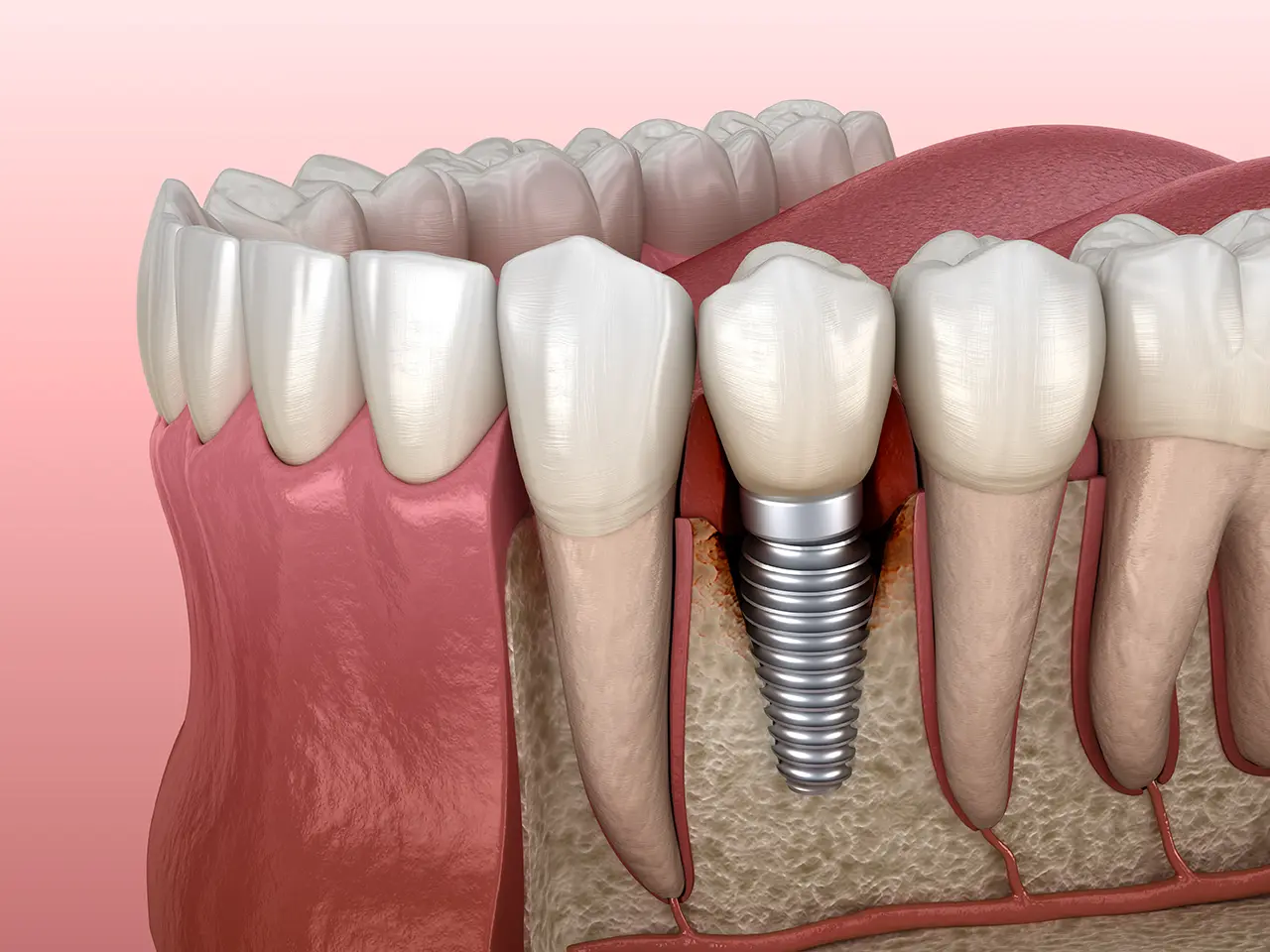
- 2-3 days after placement in the jawbone, osteoblasts begin to grow into the micro-rough surface of the implant.
- By the 4th-6th day, they connect with the trabeculae - cells of the spongy bone of the alveolar process, and with the osteons - cells of the compact bone. A bone matrix forms around the titanium post, increasing in density each day.
- In the first 2-3 weeks, spongy bone forms around the implant. It is not yet fully stable, and the newly formed bone is loose. Chewing forces on the new root are not recommended.
- Over the next 2-4 months, dense bone forms. During this period, the primary stability of the post is maintained, and it can be loaded with a permanent structure.
- After 5-6 months, the artificial root fully integrates with the jawbone. The gap disappears - a strong mature bone forms. Proper care of the new tooth will make it an integral part of the dental system within a year.
Factors influencing successful implant integration:
- Quality of the inserted structure (material, special coatings).
- Density of the patient's jawbone, their age, and health status.
- Meticulous adherence to the dental implantation protocol by the dentist.
- Compliance with instructions by the patient during the rehabilitation period.
Reasons for Implant Integration Failure
Dentist Errors
- Overheating of the bone.
When preparing the site for the titanium root, the dentist may use blunt instruments. Worse, if adequate cooling is neglected during surgery. This leads to the death of the bone section. The artificial root cannot merge with the bone. - Insufficient sterility of the oral cavity.
Before implantation, teeth are cleaned of plaque and tartar, caries and pulpitis are treated, and inflammations are eliminated. The dentist may overlook something or fail to detect hidden problems (e.g., a cyst next to the placement site). Remaining infection can cause inflammation and prevent integration. - Incorrect choice of implant site.
If the titanium root is placed in an area with insufficient bone, it can become unstable. - Ignoring relative contraindications.
The implant may not integrate if the operation is performed before eliminating contraindications, such as not waiting for blood sugar levels to normalize in diabetes cases.
Patient Errors
- Disregarding postoperative instructions.
Violating recommendations during the rehabilitation period: visiting saunas/baths, flying, physical activities, ignoring prescribed medications. - Refusing preventative check-ups.
This hinders monitoring of integration and timely detection of issues.
Reasons for Implant Rejection
Errors by Professionals
- Implant overload.
A crown on the artificial root can cause an incorrect bite. This is an orthodontist's mistake. Constant overload can lead to rejection. - Planning errors.
Causes of peri-implantitis include:
- placement too close to another tooth or implant;
- thin gum tissue unable to protect the area from infection;
- insufficient gum volume around the implant, leading to mobility and peri-implantitis.
- Prosthesis errors.
A weak connection between the abutment and implant or crown can lead to infections. Cement residues after crown fixation can also cause problems. An incorrectly selected prosthetic construction can create additional stress.
Patient Errors
- Inadequate care.
Artificial teeth require the same care as natural ones. Poor oral hygiene can lead to bacterial accumulation and the development of mucositis, threatening the loss of connection between the implant and tissues. In the mucositis stage, the implant can still be saved, but in peri-implantitis, when the inflammation affects and destroys the bone, it must be removed. - Smoking.
Nicotine impairs the function of salivary glands and promotes the growth of pathogens, increasing the risk of gum and bone inflammation around the implant, leading to peri-implantitis. Nicotine also constricts blood vessels, limiting nutrient supply to the tissues.
Systemic diseases require special preparation before implantation. An exacerbation after surgery can cause rejection of the artificial root. It's important to monitor chronic diseases to avoid exacerbations.
The success of implantation depends equally on professionals and patients. A responsible attitude to their duties before and after the procedure guarantees satisfaction with the results.
How Does Implant Rejection Occur?
There are three stages:
- In the first six months, the implant may not integrate due to inflammation, allergies, or the risk of mucositis.
- After 1-2 years, rejection of the titanium root can occur due to excessive loads, poor oral hygiene, or bad habits.
- After 3-5 years, rejection may happen because of issues with the endocrine system, flare-ups of chronic diseases, or jaw diseases.
During rehabilitation, it's important to follow the doctor's advice and not skip check-ups. This can help identify and treat inflammation in time, preventing implant rejection.
Symptoms of Rejection
After implantation, it's important to monitor oneself. Signs that indicate rejection include:
- Pain while chewing;
- Persistent sharp pain or increasing gum swelling on the 4th or 5th day;
- High temperature (above 38°C);
- Pus discharge from the surgical wound (accompanied by an unpleasant mouth odor);
- Mobility of the root.
Comparison table
| Symptom | Normal | Complication |
|---|---|---|
| Swelling | Swelling and redness decrease by the 2nd-3rd day. | Swelling does not decrease on the 3rd day and increases. |
| Bleeding | Serous fluid is released on the first day. | Bleeding on the 2nd-3rd day after surgery. |
| Pain | Pain is felt for the first 3 days. | Severe pain on the 5th-7th day. |
| Body temperature | Temperature up to 38°C for 1-2 days. | Temperature above 38°C for more than three days. |
| Pus | No pus. | Discharge of pus with an unpleasant mouth odor. |
| Gum color | Gum redness. | Gums are blue. |
| Mobility of the tooth | The tooth is immobile. | The tooth is mobile with the exposure of the neck. |
If symptoms disappear within 3-5 days after surgery, there is no cause for concern – this is a normal response to the surgical intervention. If symptoms do not subside by the 5th day or worsen, an urgent visit to the doctor is required.
Peri-implantitis – What Is It?
- Peri-implantitis is an inflammation caused by bacteria around the implant, affecting both the gum and the bone.
- At an early stage, when bone loss is up to 3 mm, the inflammation can be stopped with conservative treatment. If the implant is still firm, the doctor will start treatment. The slightest movement is a reason for removal.
- At a middle stage, nearly half of the bone height is lost. In this case, pus is released around the root.
- At a late stage, the bone is almost completely atrophied. The formation of deep pockets exacerbates the infection.
What to Do If Rejection Begins?
- The sooner you consult an implantologist, the better the chances of saving the implant. After diagnosis, the doctor will determine the cause of rejection and the treatment method.
- In the case of mucositis, the doctor cleans the surface of the root, removes plaque, and prescribes antibiotics. In most cases, the implant can be saved.
- In the case of peri-implantitis, treatment depends on the stage. At an early stage, affected tissues are removed and antibiotics are prescribed. At a middle stage, granulations are cleaned and the bone is restored. In a severe stage, the implant is removed and the tissue is rebuilt.
How Doctors Reduce the Risk of Implant Rejection
- Use of state-of-the-art implant systems.
- Conducting a thorough examination before insertion. Bone is analyzed using computer tomography.
- Eliminating all inflammation in the oral cavity. The implant placement is selected in the program, and a 3D model of the denture is created.
- Using only sterile instruments. Implants are taken out of sterile packaging right before insertion.
- Monitoring osseointegration and planning preventive examinations to detect and treat problems early.
Preventing Implant Rejection
- Only go to licensed clinics equipped with modern technology and staffed by experienced doctors.
- Do not hide any chronic diseases or bad habits from your doctor.
- Follow all the doctor's recommendations during rehabilitation.
- Pay attention to oral hygiene. Use an irrigator, brush your teeth regularly.
- If complications arise, consult a doctor immediately.
- Keep chronic diseases under control.
Repeated Implantation After Rejection
Replacing a rejected implant with a new one is possible. The procedure involves several steps: removal of the crown, removal of the implant, treating the cause of rejection, antibiotic therapy, osteoplasty, crown adjustment, and placing a new root after healing.
Frequently Asked Questions
How common is dental implant rejection?
Dental implant rejection is relatively rare, with the success rate of operations usually exceeding 90%. Factors influencing the success rate include the patient's overall health, the quality of the jawbone, adherence to postoperative care instructions, and the dentist's skill.
Is the rejection of a dental implant painful?
Rejection of a dental implant can be accompanied by pain or discomfort, especially if an infection is present. However, not all implant rejections cause severe pain. Some signs of rejection, like a loosened implant, may not immediately cause pain. Any discomfort or unusual symptoms around the implant should prompt a visit to the dentist.
What is the difference between rejection and failure of an implant?
Implant rejection means that the body's immune response negatively affects the implant's integration, which is quite rare. Implant failure, more commonly, refers to the implant's inability to osseointegrate (properly bond with the bone) or maintain this bond over time, often due to infection, insufficient bone density, or excessive force on the implant.









